Page 1 of 1
The Affordable Care Act (ACA) created PCORI to help patients, clinicians, payers and the public make informed health decisions by advancing comparative effectiveness research. PCORI’s research is to be funded, in part, by fees paid by either health insurers or sponsors of self-insured health plans. These fees are widely known as PCORI fees. Health insurers and self-insured plan sponsors are required to report and pay PCORI fees annually using IRS Form 720 (Quarterly Federal Excise Tax Return). The report and fees are due on July 31st with respect to the plan year that ended during the preceding calendar year. For instance, for calendar year plans, the fee that is due July 31, 2018 applies to the plan year that ended December 31, 2017.
Reporting PCORI fees on Form 720
Form 720 and completion instructions are posted on the IRS’ website. Insurers and self-insured plan sponsors must report the average number of lives covered under the plan. For fully insured plans, the carrier is responsible for reporting and paying the fee on the employers behalf. For a self-insured plan, the plan sponsor (employer) enters information for “self-insured health plans.” The number of covered lives is then multiplied by the applicable rate based on the plan year end date. Form 720 that is due July 31, 2018, will reflect payment for plan years ending in 2017. The applicable rate depends on the plan year end date:
The applicable rate may increase for inflation in future years. However, the program ends in 2019 and PCORI fees will not apply for plan years ending after September 30, 2019. Insurers or self-insured plan sponsors that file Form 720 only for the purpose of reporting PCORI fees do not need to file Form 720 for the first, third or fourth quarter of the year. Insurers or self-insured plan sponsors that file Form 720 to report quarterly excise tax liability (for example, to report the foreign insurance tax) should enter a PCORI fee amount only on the second quarter filing. See below for more information about affected plans and methods for calculating the number of participants and amount of the required PCORI fee.
(more…)
The Affordable Care Act added a patient-centered outcomes research (PCOR) fee on health plans to support clinical effectiveness research. The PCOR fee applies to plan years ending on or after Oct. 1, 2012, and before Oct. 1, 2019. The PCOR fee is due by July 31 of the calendar year following the close of the plan year. For plan years ending in 2014, the fee is due by July 31, 2015.
PCOR fees are required to be reported annually on Form 720, Quarterly Federal Excise Tax Return, for the second quarter of the calendar year. The due date of the return is July 31. Plan sponsors and insurers subject to PCOR fees but not other types of excise taxes should file Form 720 only for the second quarter, and no filings are needed for the other quarters. The PCOR fee can be paid electronically or mailed to the IRS with the Form 720 using a Form 720-V payment voucher for the second quarter. According to the IRS, the fee is tax-deductible as a business expense.
The PCOR fee is assessed based on the number of employees, spouses and dependents that are covered by the plan. The fee is $1 per covered life for plan years ending before Oct. 1, 2013, and $2 per covered life thereafter, subject to adjustment by the government. For plan years ending between Oct. 1, 2014, and Sept. 30, 2015, the fee is $2.08. The Form 720 instructions are expected to be updated soon to reflect this increased fee.
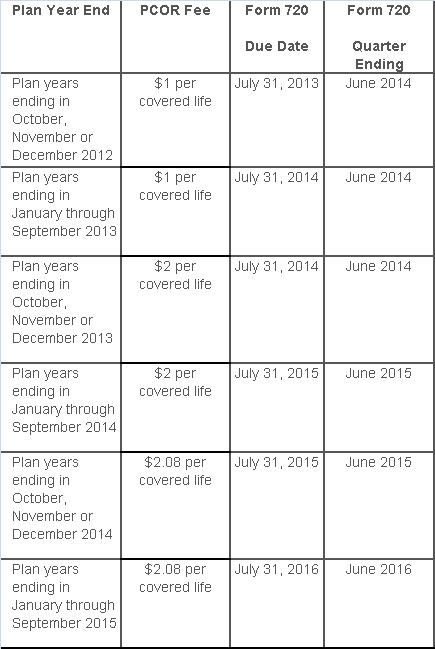
This chart summarizes the fee schedule based on the plan year end and shows the Form 720 due date. It also contains the quarter ending date that should be reported on the first page of the Form 720 (month and year only per IRS instructions). The plan year end date is not reported on the Form 720.
For insured plans, the insurance company is responsible for filing Form 720 and paying the PCOR fee. Therefore, employers with only fully- insured health plans have no filing requirement.
If an employer sponsors a self-insured health plan, the employer must file Form 720 and pay the PCOR fee. For self-insured plans with multiple employers, the named plan sponsor is generally required to file Form 720. A self-insured health plan is any plan providing accident or health coverage if any portion of such coverage is provided other than through an insurance policy.
Since the fee is a tax assessed against the plan sponsor and not the plan, most funded plans subject to ERISA must not pay the fee using plan assets since doing so would be considered a prohibited transaction by the U.S. Department of Labor (DOL). The DOL has provided some limited exceptions to this rule for plans with multiple employers if the plan sponsor exists solely for the purpose of sponsoring and administering the plan and has no source of funding independent of plan assets.
Plans sponsored by all types of employers, including tax-exempt organizations and governmental entities, are subject to the PCOR fee. Most health plans, including major medical plans, prescription drug plans and retiree-only plans, are subject to the PCOR fee, regardless of the number of plan participants. The special rules that apply to Health Reimbursement Accounts (HRAs) and Health Flexible Spending Accounts (FSAs) are discussed below.
Plans exempt from the fee include:
If a plan sponsor maintains more than one self-insured plan, the plans can be treated as a single plan if they have the same plan year. For example, if an employer has a self-insured medical plan and a separate self-insured prescription drug plan with the same plan year, each employee, spouse and dependent covered under both plans is only counted once for purposes of the PCOR fee.
The IRS has created a helpful chart showing how the PCOR fee applies to common types of health plans.
Health Reimbursement Accounts (HRAs) - Nearly all HRAs are subject to the PCOR fee because they do not meet the conditions for exemption. An HRA will be exempt from the PCOR fee if it provides benefits only for dental or vision expenses, or it meets the following three conditions:
Health Flexible Spending Accounts (FSAs) - A health FSA is exempt from the PCOR fee if it satisfies an availability condition and a maximum benefit condition.
Additional special rules for HRAs and FSAs . Once an employer determines that its HRA or FSA is subject to the PCOR fee, the employer should consider the following special rules:
The IRS provides different rules for determining the average number of covered lives (i.e., employees, spouses and dependents) under insured plans versus self-insured plans. The same method must be used consistently for the duration of any policy or plan year. However, the insurer or sponsor is not required to use the same method from one year to the next.
A plan sponsor of a self-insured plan may use any of the following three
methods to determine the number of covered lives for a plan year:
1. Actual count method. Count the covered lives on each day of the plan year and divide by the number of days in the plan year.
Example: An employer has 900 covered lives on Jan. 1, 901 on Jan. 2, 890 on
Jan. 3, etc., and the sum of the lives covered under the plan on each day of
the plan year is 328,500. The average number of covered lives is 900 (328,500 ÷
365 days).
2. Snapshot method. Count the covered lives on a single day in each quarter (or more than one day) and divide the total by the number of dates on which a count was made. The date or dates must be consistent for each quarter. For example, if the last day of the first quarter is chosen, then the last day of the second, third and fourth quarters should be used as well.
Example: An employer has 900 covered lives on Jan. 15, 910 on April 15, 890 on
July 15, and 880 on Oct. 15. The average number of covered lives is 895 [(900 +
910+ 890+ 880) ÷ 4 days].
As an alternative to counting actual lives, an employer can count the number of
employees with self-only coverage on the designated dates, plus the number of
employees with other than self-only coverage multiplied by 2.35.
3. Form 5500 method. If a Form 5500 for a plan is filed before the due date of the Form 720 for that year, the plan sponsor can determine the number of covered lives based on the Form 5500. If the plan offers just self-only coverage, the plan sponsor adds the participant counts at the beginning and end of the year (lines 5 and 6d on Form 5500) and divides by 2. If the plan also offers family or dependent coverage, the plan sponsor adds the participant counts at the beginning and end of the year (lines 5 and 6d on Form 5500) without dividing by 2.
Example: An employer offers single and family coverage with a plan year ending
on Dec. 31. The 2013 Form 5500 is filed on June 5, 2014, and reports 132
participants on line 5 and 148 participants on line 6d. The number of covered
lives is 280 (132 + 148).
To evaluate liability for PCOR fees, plan sponsors should identify all of their plans that provide medical benefits and determine if each plan is insured or self-insured. If any plan is self-insured, the plan sponsor should take the following actions: