Page 2 of 2
Under the Affordable Care Act, (ACA) a fund for a new nonprofit corporation to assist in clinical effectiveness research was created. To aid in the financial support for this endeavor, certain health insurance carriers and health plan sponsors are required to pay fees based on the average number of lives covered by welfare benefits plans. These fees are referred to as either Patient-Centered Outcome Research Institute (PCORI) or Clinical Effectiveness Research (CER) fees.
The applicable fee was $2.26 for plan years ending on or after October 1, 2016 and before October 1, 2017. For plan years ending on or after October 1, 2017 and before October 1, 2018, the fee is $2.39. Indexed each year, the fee amount is determined by the value of national health expenditures. The fee phases out and will not apply to plan years ending after September 30, 2019.
As a reminder, fees are required for all group health plans including Health Reimbursement Arrangements (HRAs), but are not required for health flexible spending accounts (FSAs) that are considered excepted benefits. To be an excepted benefit, health FSA participants must be eligible for their employer’s group health insurance plan and may include employer contributions in addition to employee salary reductions. However, the employer contributions may only be $500 per participant or up to a dollar for dollar match of each participant’s election.
HRAs exempt from other regulations would be subject to the CER fee. For instance, an HRA that only covered retirees would be subject to this fee, but those covering dental or vision expenses only would not be, nor would employee EAPs, disease management programs and wellness programs be required to pay CER fees.
Today the IRS released Revenue Procedure 2016-55 confirming a $50 increase in the health FSA contribution limit to $2,600.
With the passing of the ACA, employee contributions to an FSA were initially limited to $2500 per plan year. This has increased since 2014 to adjust for inflation with the limit being bumped up slightly to $2550 for 2015 & 2016 plan years.
Now, for health FSA plan years beginning on or after January 1, 2017, we have a new increase in the salary reduction contribution limit to $2,600. Be sure to double-check your Section 125 cafeteria plan document to confirm that it automatically incorporates these health FSA cost-of-living increases or to see if you need to specifically request to have the cap increased.
Earlier this year, the IRS also announced the inflation adjusted amounts for 2017 HSA contributions in Revenue Procedure 2016-28. For individuals in self-only coverage, the 2017 contribution limit will increase to $3,400 (up from $3,350). The family coverage contribution limit remains at $6,750 again in 2017.
The Affordable Care Act (“ACA”), introduced in 2014 the Transitional Reinsurance Fee (“Fee”) in an effort to fund reinsurance payments to health insurance issuers that cover high-risk individuals in the individual market and to stabilize insurance premiums in the market for the 2014 through 2016 years. The Fee has also been instituted to pay administrative costs related to the Early Retiree Reinsurance Program.
BACKGROUND ON TRANSITIONAL REINSURANCE PROGRAM
The ACA established a transitional reinsurance program to provide payments to health insurance issuers that cover high risk individuals in an attempt to evenly spread the financial risk of issuers. The program is designed to provide issuers with greater payment stability as insurance market reforms are implemented and the state-based health insurance exchanges/marketplaces facilitate increased enrollment. It is expected that the program will reduce the uncertainty of insurance risk in the individual market by partially offsetting issuers’ risk associated with high-cost enrollees. In an effort to fund the program, the ACA created the Fee which is a temporary fee that is assessed on health insurance issuers and plan sponsors of self-funded health plans. The Fee is applicable for the 2014, 2015 and 2016 years and is deductible as an ordinary and necessary business expense.
The Fee is generally applicable to all health insurance plans providing major medical coverage including sponsors of self-insured group health plans. Major medical coverage is defined as health coverage for a broad range of services and treatments, including diagnostic and preventive services, as well as medical and surgical conditions in inpatient, outpatient and emergency room settings. Since COBRA continuation coverage generally qualifies as major medical coverage, the Fee will also apply in this instance. It does not, however, apply to employer provided major medical coverage that is secondary to Medicare.
The Fee, as currently structured, does not apply to various other types of plans including (but not limited to) health savings accounts (H.S.A.s), employee assistance plans (EAP) or wellness programs that do not provide major medical coverage, health reimbursement arrangements integrated with a group health plan (HRA), health flexible spending accounts (FSA) and coverage that consists of only excepted benefits (e.g. stand-alone dental and vision).
AMOUNT OF THE FEE
The Fee for the 2015 benefit year is equal to $44 per covered life. It is expected that the Fee for the 2015 benefit year will generate approximately $8 billion in revenue. The Fee for the 2016 year is expected to be $27 per covered life and will raise approximately $5 billion in revenue. Thereafter, the Fee is set to expire and no longer be applicable. The fee for 2014 was $63 per covered life.
REPORTING THE NUMBER OF COVERED LIVES AND PAYING THE FEE
The 2015 ACA Transitional Reinsurance Program Annual Enrollment and Contributions Submission Form will be available on www.pay.gov on October 1, 2015. The form for 2014 is also available on this website. Please note there is a separate form for each benefit year. For the 2015 year, the number of covered lives must be reported to the Department no later than November 16, 2015. The Department will then notify reporting organizations no later than December 15, 2015 the amount of the fee that will be due and payable.
As with the 2014 benefit year, the Department of Health and Human Services has given contributing entities two different options to make the payment. Under the first option, the first portion of the Fee ($33 per covered life) is due and payable no later than January 15, 2016 (30 days after issuance of the notice from the Department). This portion of the Fee will cover reinsurance payments and administrative expenses. The second portion of the Fee ($11 per covered life) will cover Treasury’s administrative costs associated with the Early Retiree Reinsurance Program and will be due no later than November 15, 2016.
Under the second payment option, contributing entities can opt to pay the full amount ($44 per covered life) by January 15, 2016.
As the number of covered lives is due to be reported no later than November 16th of this year, employers should review their types of health coverage and determine which plans are subject to the Fee. Employers that have fully insured plans should be on the lookout for potential increased premiums as the insurance carrier is responsible to report and pay the Fee on behalf of the plan in these instances. Those with self funded medical coverage need to be sure to report and pay the fe
The Affordable Care Act added a patient-centered outcomes research (PCOR) fee on health plans to support clinical effectiveness research. The PCOR fee applies to plan years ending on or after Oct. 1, 2012, and before Oct. 1, 2019. The PCOR fee is due by July 31 of the calendar year following the close of the plan year. For plan years ending in 2014, the fee is due by July 31, 2015.
PCOR fees are required to be reported annually on Form 720, Quarterly Federal Excise Tax Return, for the second quarter of the calendar year. The due date of the return is July 31. Plan sponsors and insurers subject to PCOR fees but not other types of excise taxes should file Form 720 only for the second quarter, and no filings are needed for the other quarters. The PCOR fee can be paid electronically or mailed to the IRS with the Form 720 using a Form 720-V payment voucher for the second quarter. According to the IRS, the fee is tax-deductible as a business expense.
The PCOR fee is assessed based on the number of employees, spouses and dependents that are covered by the plan. The fee is $1 per covered life for plan years ending before Oct. 1, 2013, and $2 per covered life thereafter, subject to adjustment by the government. For plan years ending between Oct. 1, 2014, and Sept. 30, 2015, the fee is $2.08. The Form 720 instructions are expected to be updated soon to reflect this increased fee.
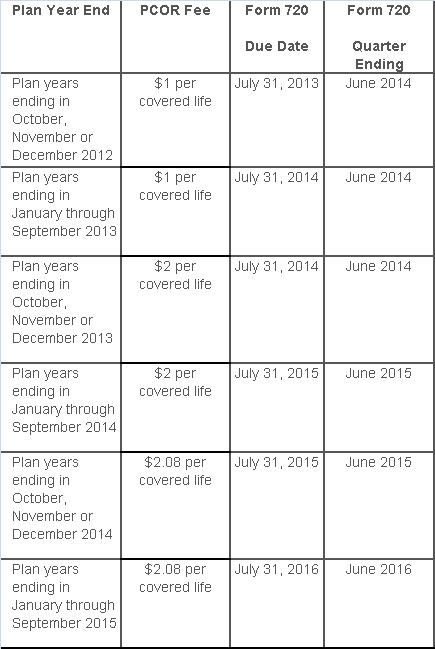
This chart summarizes the fee schedule based on the plan year end and shows the Form 720 due date. It also contains the quarter ending date that should be reported on the first page of the Form 720 (month and year only per IRS instructions). The plan year end date is not reported on the Form 720.
For insured plans, the insurance company is responsible for filing Form 720 and paying the PCOR fee. Therefore, employers with only fully- insured health plans have no filing requirement.
If an employer sponsors a self-insured health plan, the employer must file Form 720 and pay the PCOR fee. For self-insured plans with multiple employers, the named plan sponsor is generally required to file Form 720. A self-insured health plan is any plan providing accident or health coverage if any portion of such coverage is provided other than through an insurance policy.
Since the fee is a tax assessed against the plan sponsor and not the plan, most funded plans subject to ERISA must not pay the fee using plan assets since doing so would be considered a prohibited transaction by the U.S. Department of Labor (DOL). The DOL has provided some limited exceptions to this rule for plans with multiple employers if the plan sponsor exists solely for the purpose of sponsoring and administering the plan and has no source of funding independent of plan assets.
Plans sponsored by all types of employers, including tax-exempt organizations and governmental entities, are subject to the PCOR fee. Most health plans, including major medical plans, prescription drug plans and retiree-only plans, are subject to the PCOR fee, regardless of the number of plan participants. The special rules that apply to Health Reimbursement Accounts (HRAs) and Health Flexible Spending Accounts (FSAs) are discussed below.
Plans exempt from the fee include:
If a plan sponsor maintains more than one self-insured plan, the plans can be treated as a single plan if they have the same plan year. For example, if an employer has a self-insured medical plan and a separate self-insured prescription drug plan with the same plan year, each employee, spouse and dependent covered under both plans is only counted once for purposes of the PCOR fee.
The IRS has created a helpful chart showing how the PCOR fee applies to common types of health plans.
Health Reimbursement Accounts (HRAs) - Nearly all HRAs are subject to the PCOR fee because they do not meet the conditions for exemption. An HRA will be exempt from the PCOR fee if it provides benefits only for dental or vision expenses, or it meets the following three conditions:
Health Flexible Spending Accounts (FSAs) - A health FSA is exempt from the PCOR fee if it satisfies an availability condition and a maximum benefit condition.
Additional special rules for HRAs and FSAs . Once an employer determines that its HRA or FSA is subject to the PCOR fee, the employer should consider the following special rules:
The IRS provides different rules for determining the average number of covered lives (i.e., employees, spouses and dependents) under insured plans versus self-insured plans. The same method must be used consistently for the duration of any policy or plan year. However, the insurer or sponsor is not required to use the same method from one year to the next.
A plan sponsor of a self-insured plan may use any of the following three
methods to determine the number of covered lives for a plan year:
1. Actual count method. Count the covered lives on each day of the plan year and divide by the number of days in the plan year.
Example: An employer has 900 covered lives on Jan. 1, 901 on Jan. 2, 890 on
Jan. 3, etc., and the sum of the lives covered under the plan on each day of
the plan year is 328,500. The average number of covered lives is 900 (328,500 ÷
365 days).
2. Snapshot method. Count the covered lives on a single day in each quarter (or more than one day) and divide the total by the number of dates on which a count was made. The date or dates must be consistent for each quarter. For example, if the last day of the first quarter is chosen, then the last day of the second, third and fourth quarters should be used as well.
Example: An employer has 900 covered lives on Jan. 15, 910 on April 15, 890 on
July 15, and 880 on Oct. 15. The average number of covered lives is 895 [(900 +
910+ 890+ 880) ÷ 4 days].
As an alternative to counting actual lives, an employer can count the number of
employees with self-only coverage on the designated dates, plus the number of
employees with other than self-only coverage multiplied by 2.35.
3. Form 5500 method. If a Form 5500 for a plan is filed before the due date of the Form 720 for that year, the plan sponsor can determine the number of covered lives based on the Form 5500. If the plan offers just self-only coverage, the plan sponsor adds the participant counts at the beginning and end of the year (lines 5 and 6d on Form 5500) and divides by 2. If the plan also offers family or dependent coverage, the plan sponsor adds the participant counts at the beginning and end of the year (lines 5 and 6d on Form 5500) without dividing by 2.
Example: An employer offers single and family coverage with a plan year ending
on Dec. 31. The 2013 Form 5500 is filed on June 5, 2014, and reports 132
participants on line 5 and 148 participants on line 6d. The number of covered
lives is 280 (132 + 148).
To evaluate liability for PCOR fees, plan sponsors should identify all of their plans that provide medical benefits and determine if each plan is insured or self-insured. If any plan is self-insured, the plan sponsor should take the following actions:
On December 22, 2014, the Departments of Health and Human Services (HHS) issued proposed regulations for changes to the Summary of Benefits and Coverage (SBC).
The proposed regulations clarify when and how a plan administrator or insurer must provide an SBC, shortens the SBC template, adds a third cost example, and revises the uniform glossary. The proposed regulations provide new information and also incorporate several FAQs that have been issued since the final SBC regulations were issued in 2012.
These proposed changes are effective for plan years and open enrollment period beginning on or after September 1, 2015. Comments on the proposed regulations will be accepted until March 2,2015 and are encourages on many of the provisions.
New Template
The new SBC template eliminates a significant amount of information that the Departments characterized as not being required by law and/or as having been identified by consumer testing as less useful for choosing coverage.
The sample completed SBC template for a standard group health plan has been reduced from four double-sided pages to two-and-a-half double-sided pages. Some of the other changes include:
Glossary Revisions
Revisions to the uniform glossary have also been proposed. The glossary must be available to plan participants upon request. Some definitions have been changed and new medical terms such as claim, screening, referral and specialty drug have been added. Additional terms related to health care reform such as individual responsibility requirement, minimum value and cost-sharing reductions have also been added.
Paper vs Electronic Distribution
SBCs may continue to be provided electronically to group plan participants in connection with their online enrollment or online renewal of coverage. SBCs may also be provided electronically to participants who request an SBC online. These individuals must also have the option to receive a paper copy upon request.
SBCs for self-insured non-federal government plans may continue to be provided electronically if the plan conforms to either the electronic distribution requirements that apply ERISA plan or the rules that apply to individual health insurance coverage.
Types of Plans to Which SBCs Apply
The regulations confirm that SBCs are not required for expatriate health plans, Medicare Advantage plans or plans that qualify as excepted benefits. Excepted benefits include:
SBCs are required for:
The IRS and Social Security Administration released the 2015 cost-of-living (COLA) adjustments that apply to health flexible spending accounts (FSAs) in Revenue Procedure 2014-61. The new annual limit for health FSAs, including general-purpose and limited-purpose health FSAs, is $2,550 for plan years starting on or after January 1, 2015.
The $2,550 limit is prorated for short plan years (plan years that are shorter than 12 months) and any carry over amount from participants’ previous plan years may be added to the limit. For instance, participants may elect $2,550 for the 2015 plan year and carry over a maximum of $500 from the previous plan year, making their total account value $3,050 for the 2015 plan year. In other words, the $500 carryover does not count against or affect the $2,550 salary reduction limit. Please note that an employer must decide to allow to either offer participants a option of a max $500 carryover OR the 2.5 month extension to use funds. An employer can not offer both options under their plan.
On October 31, 2013, the US Treasury and the IRS issued Notice 2013-71, which modifies the “use it or lose it” rule for Healthcare Flexible Spending Accounts (FSAs).
A Healthcare FSA is a form of cafeteria plan benefit offered by employers to allow their employees to pay for eligible out of pocket healthcare expenses with pre-tax dollars. Healthcare FSAs are typically funded by salary reduction contributions. Effective for plan years beginning after December 31, 2012, and employee’s contributions to a Healthcare FSA are limited to $2500 per year (indexed for inflation beginning in 2014).
Historically, these contributions were also subject to a “use it or lose it” rule which provided that contribution to plan that are not used before the end of the plan’s fiscal year would be forfeited. This rule was modified several years ago to permit a plan to add a “grace period” of 2 ½ months following the end of the plan’s fiscal year to allow employees an extra amount of time to use their FSA funds before losing them.
The new rules issued by the IRS permit another option that employers may want to consider. An employer may amend its plan document to permit a carryover of up to $500 for any unused FSA funds at the end of the plan year. The carryover, if permitted in the plan, may be used to pay medical expenses incurred during the plan year to which it is carried over, and would be in addition to the $2500 employee contribution limit.
A plan adopting the new carryover option is not permitted to also provide a grace period. An employer must decide to either provide a grace period or the new carryover option, but not both. Of course, an employer may choose to provide for a carryover limit of less than $500, or not to permit the carryover or grace period at all, as these are both entirely optional. When deciding whether or not to eliminate a grace period in favor of the new carryover option, an employer may want to compare the potential administrative impact of each option.
As mentioned above, the new carryover rule is not available during a plan year in which the plan permits a grace period. Therefore, plans containing a grace period must first be amended to remove it if the employer wants to add a carryover provision. The amendment to remove the grace period must be adopted before the end of the plan year in which it becomes effective. For example, if an employers wants to permit employees to carryover up to $500 from the 2014 plan year to the 2015 plan year, the employer must amend the plan and provide participants with notice of the amendment before the end of the 2014 plan year.
Please contact our office for more information on how to implement an FSA into your workplace or amend your existing plan document.
The Patient Protection and Affordable Care Act (the “ACA”) adds a new Section 4980H to the Internal Revenue Code of 1986 which requires employers to offer health coverage to their employees (aka the “Employer Mandate”). The following Q&As are designed to deal with commonly asked questions. These Q&As are based on proposed regulations and final regulations, when issued, may change the requirements.
Question 1: What Is the Employer Mandate?
On January 1, 2014, the Employer Mandate will requiring large employers to offer health coverage to full-time employees and their children up to age 26 or risk paying a penalty. These employers will be forced to make a choice:
OR
This “play or pay” system has become known as the Employer Mandate. The January 1, 2014 effective date is deferred for employers with fiscal year plans that meet certain requirements.
Only “large employers” are required to comply with this mandate. Generally speaking, “large employers” are those that had an average of 50 or more full-time or full-time equivalent employees on business days during the preceding year. “Full-time employees” include all employees who work at least 30 hours on average each week. The number of “full-time equivalent employees” is determined by combining the hours worked by all non-full-time employees.
To “play” under the Employer Mandate, a large employer must offer health coverage that is:
This includes coverage under an employer-sponsored group health plan, whether it be fully insured or self-insured, but does not include stand-alone dental or vision coverage, or flexible spending accounts (FSA).
Coverage is considered “affordable” if an employee’s required contribution for the lowest-cost self-only coverage option does not exceed 9.5% of the employee’s household income. Coverage provides “minimum value” if the plan’s share of the actuarially projected cost of covered benefits is at least 60%.
If a large employer does not “play” for some or all of its full-time employees, the employer will have to pay a penalty, as shown in following two scenarios.
Scenario #1- An employer does not offer health coverage to “substantially all” of its full-time employees and any one of its full-time employees both enrolls in health coverage offered through a State Insurance Exchange, which is also being called a Marketplace (aka an “Exchange”), and receives a premium tax credit or a cost-sharing subsidy (aka “Exchange subsidy”).
In this scenario, the employer will owe a “no coverage penalty.” The no coverage penalty is $2,000 per year (adjusted for inflation) for each of the employer’s full-time employees (excluding the first 30). This is the penalty that an employer should be prepared to pay if it is contemplating not offering group health coverage to its employees.
Scenario #2- An employer does provide health coverage to its employees, but such coverage is deemed inadequate for Employer Mandate purposes, either because it is not “affordable,” does not provide at least “minimum value,” or the employer offers coverage to substantially all (but not all) of its full-time employees and one or more of its full-time employees both enrolls in Exchange coverage and receives an Exchange subsidy.
In this second scenario, the employer will owe an “inadequate coverage penalty.” The inadequate coverage penalty is $3,000 per person and is calculated, based not on the employer’s total number of full-time employees, but only on each full-time employee who receives an Exchange subsidy. The penalty is capped each month by the maximum potential “no coverage penalty” discussed above.
Because Exchange subsidies are available only to individuals with household incomes of at least 100% and up to 400% of the federal poverty line (in 2013, a maximum of $44,680 for an individual and $92,200 for a family of four), employers that pay relatively high wages may not be at risk for the penalty, even if they fail to provide coverage that satisfies the affordability and minimum value requirements.
Exchange subsidies are also not available to individuals who are eligible for Medicaid, so some employers may be partially immune to the penalty with respect to their low-wage employees, particularly in states that elect the Medicaid expansion. Medicaid eligibility is based on household income. It may be difficult for an employer to assume its low-paid employees will be eligible for Medicaid and not eligible for Exchange subsidies as an employee’s household may have more income than just the wages they collect from the employer. But for employers with low-wage workforces, examination of the extent to which the workforce is Medicaid eligible may be worth exploring.
Exchange subsidies will also not be available to any employee whose employer offers the employee affordable coverage that provides minimum value. Thus, by “playing” for employees who would otherwise be eligible for an Exchange subsidy, employers can ensure they are not subject to any penalty, even if they don’t “play” for all employees.
Beginning in 2013, employee pre-tax contributions to a flexible spending account (FSA) will be limited to $2500. In the past, companies could impose their own limits on these employee contributions.
The limit applies based on your cafeteria plan’s plan year. It is first applicable to plan years beginning in 2013. For the majority of companies, this means it will become effective January 1, 2013 and the open enrollment materials for 2013 have to be changed to incorporate the limit.
If the cafeteria plan utilizes the 2 ½ month grace period that allows for a carryover of amounts, these carryover amounts do not reduce the $2500 limit.
Any company contributions made to the cafeteria plan- so called “flex credits”- are not subject to any limit and do not count towards the $2500.
The $2500 is indexed for inflation, like so many other limits on benefits.
The cafeteria plan has be amended no later than December 31, 2014 to reflect the new limit.
Please be sure to consult with your current Section 125 administrator regarding updating your plan document to reflect the new FSA limit or contact our office regarding setting up an FSA account or amending your document.